What is Lipohypertrophy?
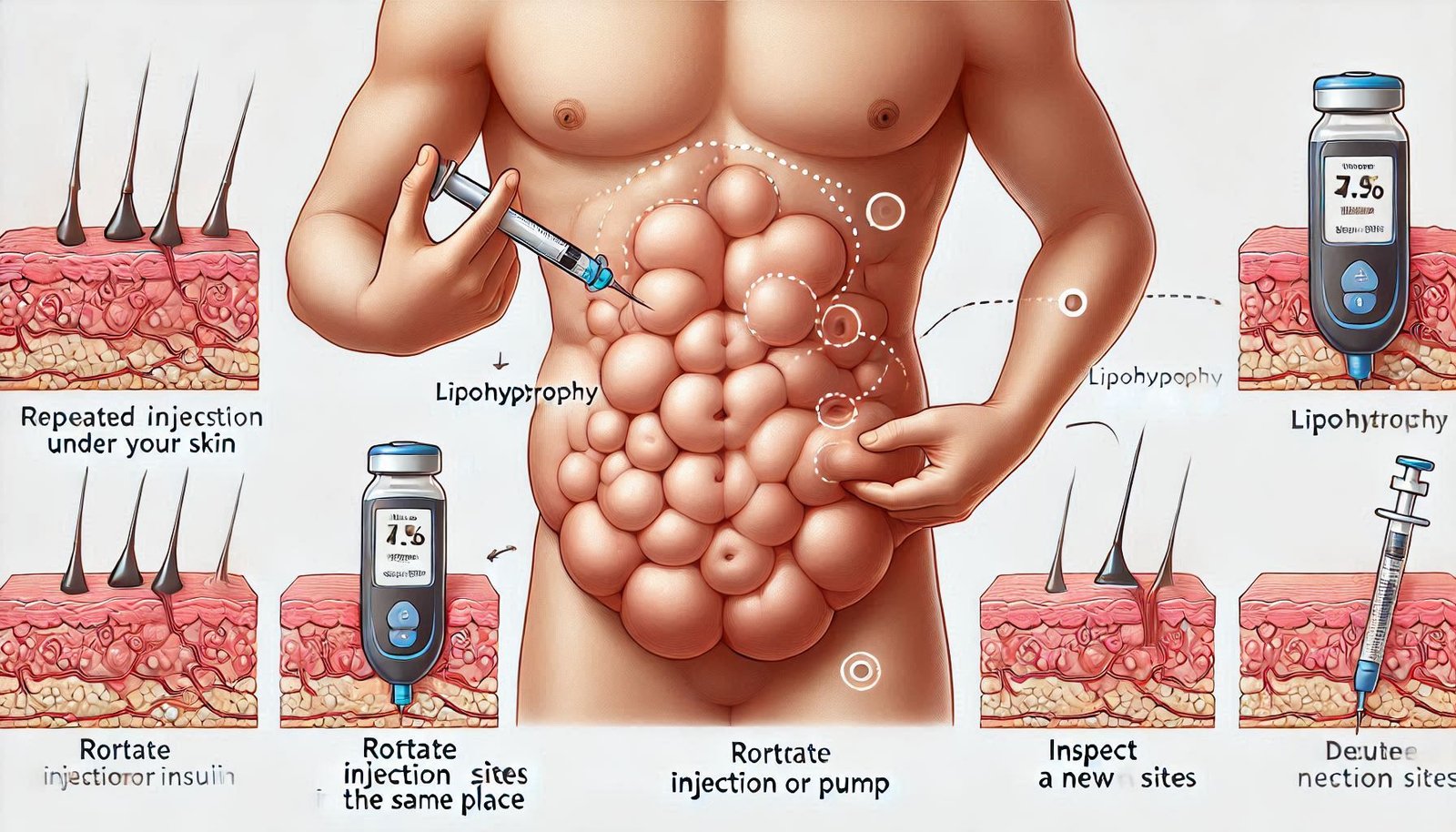
Lipohypertrophy is a condition that manifests as an abnormal accumulation of fatty tissue, resulting in noticeable lumps or bumps beneath the skin. This phenomenon often occurs due to repeated injections in the same anatomical area, essentially leading to localized fat growth. It is particularly prevalent among individuals with diabetes who utilize insulin therapy, as frequent injections in the same site can stimulate abnormal adipose tissue development.
The pathophysiology behind lipohypertrophy is tied to the body’s response to repeated trauma and insulin injection. Over time, when a person continues to inject insulin into the same site, the body may react by accumulating fat in that area. This condition is characterized not only by physical changes but can also affect the absorption and efficacy of insulin. In cases where lipohypertrophy is present, the injected insulin may not be absorbed consistently, leading to fluctuations in blood glucose levels, which further complicates diabetes management.
Prevalence studies show that lipohypertrophy affects a significant percentage of insulin-dependent individuals, often underestimated due to lack of awareness. Affected individuals may not recognize the lumps as a side effect of their treatment, and many healthcare providers may fail to routinely inquire about injection sites or examine for these fatty deposits. Consequently, the condition might go unreported and untreated, perpetuating the cycle of ineffective insulin therapy. As diabetes care emphasizes the importance of optimal insulin delivery, understanding lipohypertrophy and its eventual impact on metabolic control becomes essential for both healthcare providers and patients.
How Lipohypertrophy Affects Insulin Absorption
Lipohypertrophy, characterized by the abnormal accumulation of fat in specific regions of the body, can have significant implications for a person with diabetes, particularly regarding the absorption of insulin. When insulin is injected into lipohypertrophic areas, its absorption may be altered, leading to unpredictable and inefficient drug delivery. This is primarily due to the structural changes that occur in the subcutaneous tissue, which can create a barrier that hinders the proper uptake of insulin into the bloodstream.
The physiological mechanism behind these alterations lies in the changes in blood flow and the distribution of adipose tissue. In regions affected by lipohypertrophy, reduced perfusion may slow down the absorption rate of insulin. Consequently, this can cause delayed peak insulin action times and erratic blood glucose levels. For individuals managing diabetes, these fluctuations can complicate the already challenging task of maintaining stable blood glucose concentrations.
Moreover, the use of lipohypertrophic sites for insulin injections may lead to unintended hypoglycemia or hyperglycemia. Patients may inadvertently believe they are administering an adequate dose of insulin, only to find that its effectiveness is compromised because it is not absorbed properly. Therefore, understanding the relationship between lipohypertrophy and insulin absorption is critical in diabetes management.
Healthcare professionals frequently emphasize the importance of routinely rotating injection sites to minimize the risk of lipohypertrophy, as this can help preserve insulin absorption efficiency. Additionally, educating patients about the signs of lipohypertrophy and encouraging them to monitor their injection techniques can significantly improve glycemic control. Through such measures, individuals with diabetes can better navigate the complexities of insulin therapy and enhance their overall treatment outcomes.
Common Causes of Lipohypertrophy in Diabetes
Lipohypertrophy, a condition characterized by the abnormal accumulation of fat at insulin injection sites, poses various challenges for individuals managing diabetes. Understanding the common causes of lipohypertrophy is crucial for preventing its development and ensuring optimal blood glucose control. One of the primary factors contributing to this condition is the frequency and technique of insulin injections. When insulin is repeatedly injected into the same site without adequate rotation, it can lead to localized lipodystrophy. This consistent trauma and overuse of specific injection sites can disrupt normal tissue function and promote the formation of fatty lumps.
Furthermore, the type of needles used for insulin administration can significantly influence the risk of developing lipohypertrophy. For instance, using longer needles or those with larger gauges may cause more tissue trauma than shorter, finer needles. It is essential for individuals to choose the appropriate needle size and ensure they are utilizing the best technique for their body type and injection sites to minimize damage to the fat tissue. Additionally, proper injection technique—such as injecting at a 90-degree angle for subcutaneous injections—can help maintain the integrity of the tissue and reduce the likelihood of fat accumulation.
Another critical factor involved in the development of lipohypertrophy is inadequate management of injection sites. Failing to cleanse the area before injection or not allowing sufficient time for alcohol to evaporate can result in skin irritation and damage, further exacerbating the risk of lipohypertrophy. Additionally, the lack of education regarding the rotation of injection sites can contribute to this condition. By being aware of these common causes, individuals with diabetes can take proactive steps to prevent lipohypertrophy and enhance their overall diabetes management.
Recognizing the Symptoms of Lipohypertrophy
Lipohypertrophy is a diabetes-related condition characterized by the abnormal accumulation of fat tissue at insulin injection sites. Identifying the symptoms is crucial for effective diabetes management, as untreated lipohypertrophy can lead to poor glycemic control and complicate insulin therapy. One of the most common indicators of lipohypertrophy is the presence of markedly raised areas of fatty tissue adjacent to the injection site, which may appear smooth and even-rounded. Patients might notice these changes developing over time, often on the abdomen, thighs, or upper arms where injections are frequently administered.
While some swelling and tenderness around injection sites may be typical, lipohypertrophy typically presents as a more pronounced and persistent alteration in tissue texture. Affected areas may feel softer compared to surrounding skin or exhibit a noticeable difference in shape or size. Additionally, individuals may experience difficulty achieving consistent insulin absorption, resulting in erratic blood glucose levels. Users of insulin should monitor their injection sites carefully, as changes in these areas can significantly impact treatment effectiveness.
Moreover, it is advisable for individuals with diabetes to perform regular skin inspections to identify potential signs of lipohypertrophy early on. Health professionals recommend rotating injection sites to minimize the risk of developing this condition, emphasizing the need to inject insulin in varying locations consistently. It is worth noting that if any unfamiliar changes occur, such as hard lumps or an increase in the size of lumps near injection sites, a consultation with a healthcare provider is necessary for assessment. Awareness of these symptoms can lead to timely interventions and better overall management of diabetes.
Prevention Strategies for Lipohypertrophy
Preventing lipohypertrophy is crucial for individuals managing diabetes, particularly those who administer insulin through injections. One of the most effective strategies is to rotate injection sites consistently. This practice helps to ensure that the same area of skin does not experience repeated trauma from the needle, which can lead to the development of lipohypertrophy. It is advisable to create a rotation schedule to effectively cover all potential sites, such as the abdomen, thighs, and upper arms, while avoiding the immediate vicinity of any previous injection.
Additionally, using new needles for each injection plays a significant role in preventing lipohypertrophy. Reusing needles can lead to duller tips that cause more damage to the skin and underlying tissue, enhancing the risk of developing lipohypertrophy. It is important for diabetic patients to carry a sufficient supply of insulin needles to ensure they never resort to reusing them. Proper disposal of used needles is also vital; utilizing sharps containers will keep both patients and their environment safe.
Another essential component of preventing lipohypertrophy involves maintaining good skin care practices around injection sites. This includes cleaning the skin effectively prior to an injection to minimize infection risk, which can also damage tissues and potentially contribute to lipohypertrophy. Use an alcohol swab to cleanse the area and allow it to dry fully before injecting. Furthermore, moisturizing the skin can improve the overall condition of the tissue and promote healing after injections, further deterring the risks associated with lipohypertrophy.
By implementing these practical tips, individuals living with diabetes can significantly reduce their risk of developing lipohypertrophy and ensure a more effective insulin administration process. Consistency in these prevention strategies not only promotes healthier skin but also enhances the overall effectiveness of diabetes management.
Managing and Treating Lipohypertrophy
Effective management and treatment of lipohypertrophy are crucial for individuals with diabetes, as this condition can hinder insulin absorption and overall diabetes control. Addressing the issue begins with an earnest discussion with healthcare professionals. They can provide personalized strategies tailored to the patient’s specific needs, ensuring a more effective management plan for lipohypertrophy.
One of the primary recommendations is to rotate injection sites consistently. When insulin injections are administered in the same area repeatedly, it can contribute to the development of subcutaneous fat deposits. By varying the injection sites within recommended anatomical areas, patients can prevent further worsening of lipohypertrophy while improving insulin absorption. Patients might consider using a marking system to keep track of injection sites, enhancing rotation compliance.
Additionally, adopting good injection techniques is vital. Ensuring proper needle length and angle during administration can minimize the likelihood of complications. Healthcare professionals may suggest appropriate techniques for subcutaneous injection that can be beneficial for the metabolic management of diabetes.
In some cases, seeking pharmacological intervention may be necessary. Options may include switching to a different insulin formulation or delivery system, such as insulin pumps, which can help reduce the risk of lipohypertrophy by providing continuous subcutaneous insulin infusion.
Moreover, lifestyle adjustments play a significant role in managing lipohypertrophy. Regular physical activity can not only improve insulin sensitivity but may also aid in reducing the appearance of fat deposits. A balanced diet, rich in nutrients and low in processed sugars, further supports overall health and effective diabetes management.
Ultimately, the collaboration between patients and healthcare professionals is essential when managing and treating lipohypertrophy. Personalized strategies, combined with an emphasis on consistent care practices, can significantly mitigate its impact on diabetes management and enhance the quality of life for those affected.
When to Consult a Healthcare Professional
For individuals living with diabetes, regular monitoring of health conditions is essential for effective management. Lipohypertrophy, characterized by localized fat accumulation at injection sites, can emerge as a complication of insulin therapy. Recognizing when to seek medical advice regarding lipohypertrophy is crucial. Patients should consider consulting a healthcare professional if they observe noticeable changes in their skin or subcutaneous tissue post-injection. Signs such as swelling, hardness, or tissue irregularities warrant immediate discussion with a diabetes care provider.
Moreover, if patients experience discomfort, pain, or difficulty with insulin administration due to altered tissue characteristics, it is imperative to reach out to a healthcare professional. By communicating these issues promptly, individuals can collaborate with their healthcare team to explore alternative injection techniques, adjust insulin delivery methods, or modify their diabetes management strategies. Regular check-ups and evaluations by a healthcare provider play a significant role in identifying and addressing lipohypertrophy effectively.
Furthermore, during routine diabetes management visits, it is advisable for patients to discuss their injection practices and any related concerns. A healthcare professional can provide guidance on the best injection sites, educate patients on rotating injection locations, and recommend appropriate techniques to minimize the risk of developing lipohypertrophy. Catching this condition early can help mitigate its impact on diabetes management, ensuring optimal treatment outcomes.
In light of the complexities surrounding diabetes management, engaging with healthcare providers is not just recommended but necessary. Their expertise can offer insights into the management of lipohypertrophy and its implications for overall health. Therefore, patients should proactively seek guidance and assistance when they suspect the presence of lipohypertrophy or related concerns.