Understanding the Silent Threat of Diabetes
Diabetes, a chronic condition that affects how the body processes glucose, is a growing health concern worldwide. Often referred to as a “silent killer,” diabetes can develop over several years without presenting obvious symptoms, making it easy to overlook. With millions of individuals living with undiagnosed diabetes, awareness is fundamental for effective prevention and management. The complexity of this disease lies not only in its varied types, namely Type 1 and Type 2 diabetes, but also in the subtlety with which it can manifest.
Many people may be unaware that they are at risk of developing diabetes, as early warning signs can be easily dismissed. Common indicators include increased thirst, frequent urination, unexplained weight loss, fatigue, and blurred vision. These symptoms, while potentially alarming, are often attributed to stress or fatigue rather than being recognized as warning signs of a serious condition. This lack of recognition can lead to delays in diagnosis and treatment, reinforcing the need for regular health checks to monitor blood sugar levels.
Furthermore, the prediabetes stage often goes unnoticed, leaving individuals at an elevated risk of developing Type 2 diabetes. During this phase, blood sugar levels are higher than normal, yet not high enough for a diabetes diagnosis. Promoting public awareness of diabetes and its symptoms is essential in fostering a proactive approach to health. Individuals should be encouraged to engage in routine medical check-ups, especially if they have risk factors such as obesity, a sedentary lifestyle, or a family history of diabetes. Understanding this silent threat empowers individuals to take control of their health, enabling better management and significantly reducing the risk of complications associated with diabetes.
What is Diabetes?
Diabetes is a chronic medical condition characterized by the body’s inability to effectively use insulin, a hormone produced by the pancreas. Insulin plays a pivotal role in converting glucose, derived from the food we consume, into energy. When functioning properly, insulin allows glucose to enter cells, where it is utilized for various bodily functions. However, in individuals with diabetes, this process is impaired, resulting in elevated blood glucose levels that can lead to significant health complications.
There are primarily two types of diabetes: Type 1 and Type 2. Type 1 diabetes is an autoimmune condition where the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. This type typically manifests in childhood or adolescence but can occur at any age. Conversely, Type 2 diabetes is more prevalent and often develops in adults due to insulin resistance, where the body’s cells do not respond effectively to insulin. Over time, the pancreas cannot produce enough insulin to keep blood sugar levels within a normal range, leading to chronic hyperglycemia.
Maintaining adequate glucose levels is essential, as prolonged high blood sugar can damage blood vessels and nerves, increasing the risk of cardiovascular diseases, kidney failure, and vision loss. People with diabetes must actively monitor glucose levels, often requiring lifestyle modifications including dietary changes and regular physical activity. The management of diabetes not only influences physical health but also significantly impacts mental well-being, as individuals navigate the complexities of their condition. Awareness of diabetes and its ramifications on daily life is critical for proper self-care and to minimize the risk of long-term complications.
Global Diabetic Statistics
Diabetes has emerged as a significant global health concern, with current estimates indicating that over 463 million individuals are living with this chronic condition worldwide. The World Health Organization (WHO) anticipates that this figure will continue to rise, potentially affecting over 700 million people by 2045. This alarming statistic underscores the urgency of addressing diabetes as a major public health epidemic.
The demographics of diabetes reveal disparities based on age, gender, and geographical location. Notably, the prevalence is notably higher among older adults, with adults aged 65 years and above exhibiting a strikingly elevated incidence compared to younger populations. Furthermore, research shows that men are more likely to be diagnosed with diabetes than women, although this gap tends to vary across different regions.
Geographically, diabetes prevalence is heavily influenced by socioeconomic factors as well. Countries experiencing rapid urbanization and industrialization, especially in low to middle-income regions, have reported a surge in diabetes cases. This correlation can be attributed to lifestyle changes, such as decreased physical activity and increased consumption of processed foods, which have become more accessible in urban settings.
Moreover, regions like the Western Pacific and the Americas have shown particularly high rates of diabetes, often linked to dietary patterns and lifestyle behaviors endemic to these areas. In contrast, some European nations exhibit lower prevalence rates, attributed to better public health interventions and nutritional awareness.
In summary, the rising tide of diabetes presents a compelling public health challenge that transcends borders and demographics. Understanding the scale and seriousness of this health epidemic is essential to develop effective preventive measures and interventions aimed at curbing its impact on global health.
Causes of Diabetes: A Closer Look
Diabetes is a complex metabolic disorder characterized by elevated blood sugar levels. It manifests primarily in two forms: type 1 diabetes and type 2 diabetes, each with distinct causes and implications for insulin regulation. Understanding these different origins provides valuable insight into the disease and its management.
Type 1 diabetes is primarily an autoimmune condition. In this scenario, the body’s immune system mistakenly attacks the insulin-producing beta cells in the pancreas. As a result, the pancreas fails to produce sufficient insulin, a hormone that is crucial for glucose metabolism. The exact trigger for this autoimmune response remains unclear, but it often involves genetic predispositions coupled with environmental factors, such as viral infections. Consequently, individuals with type 1 diabetes require lifelong insulin therapy to manage their blood sugar levels effectively.
On the other hand, type 2 diabetes is largely influenced by lifestyle and genetic factors. This form of diabetes typically develops when the body becomes resistant to insulin, or when the pancreas fails to produce enough insulin to maintain normal glucose levels. Key lifestyle factors that contribute to the onset of type 2 diabetes include obesity, physical inactivity, poor diet, and smoking. Additionally, genetic factors play a significant role, as a family history of diabetes can elevate an individual’s risk. Notably, type 2 diabetes is often preventable; lifestyle modifications such as maintaining a healthy weight, engaging in regular exercise, and eating a balanced diet can significantly reduce the likelihood of developing this condition.
In understanding the causes of diabetes, it is essential to recognize the distinctions between type 1 and type 2 diabetes. While type 1 is primarily autoimmune in nature, type 2 is significantly influenced by modifiable risk factors, presenting opportunities for prevention and improved health outcomes.
The Impact of Lifestyle on Diabetes
Diabetes is a complex condition deeply intertwined with various lifestyle choices, particularly in areas such as diet, exercise, and weight management. Understanding the influence of these factors is crucial for effective diabetes management and for reducing the risk of developing the disease. A balanced diet rich in whole foods, including fruits, vegetables, whole grains, and lean proteins, plays a vital role in maintaining healthy blood sugar levels. By opting for nutrient-dense meals and limiting processed foods high in sugar and unhealthy fats, individuals can better regulate their blood glucose and improve overall health.
Exercise is another key component influencing diabetes management. Regular physical activity helps improve insulin sensitivity, allowing the body to use glucose more effectively. Engaging in at least 150 minutes of moderate aerobic activity each week—such as brisk walking, swimming, or cycling—can significantly enhance blood sugar control. Additionally, incorporating strength training exercises into one’s routine two to three times per week can aid in building muscle mass, which further supports metabolic health.
Weight management also holds significant importance in diabetes care. Excess body weight, particularly around the abdomen, can impair the body’s ability to regulate blood sugar levels and increase the risk of insulin resistance. Achieving and maintaining a healthy weight through balanced nutrition and regular exercise can lead to improved glycemic control, reducing the likelihood of diabetes-related complications. Adopting simple changes, such as monitoring portion sizes or being mindful of food choices, can make a notable difference in weight management.
In conclusion, the way individuals choose to live can profoundly impact their risk and management of diabetes. By focusing on a nutritious diet, staying active, and maintaining a healthy weight, one can make significant strides toward a healthier future and effectively manage diabetes.
Managing Diabetes: Tools and Strategies
Effectively managing diabetes involves an integrated approach that encompasses medication, dietary modifications, regular monitoring, and support systems. The primary objective is to maintain blood glucose levels within a target range, thereby minimizing complications associated with the condition.
Medication plays a crucial role in diabetes management. Patients may be prescribed insulin or oral medications that help regulate blood glucose levels. The choice of medication depends on the type of diabetes, its severity, and individual patient considerations. It is vital that patients adhere to the prescribed medication regimen, as it directly impacts their ability to control their diabetes effectively.
Dietary guidelines are equally important in managing diabetes. Incorporating balanced meals that focus on whole grains, vegetables, lean proteins, and healthy fats can promote steady blood sugar levels. Patients are often encouraged to consult with a registered dietitian who can provide personalized meal plans and education on carbohydrate counting. This knowledge enables individuals to make informed decisions about their food choices, ultimately empowering them to take charge of their health.
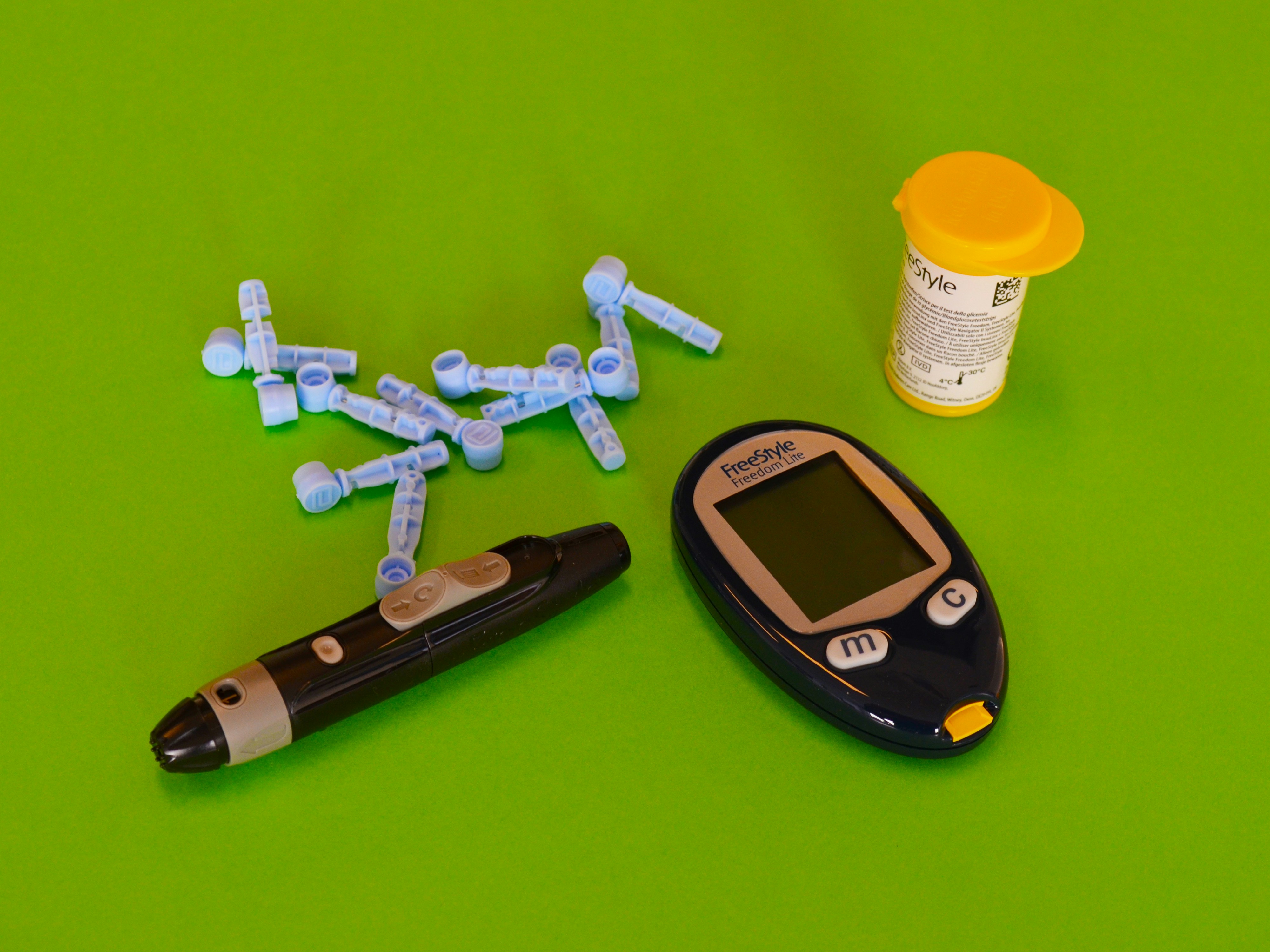
Regular monitoring of blood sugar levels is another cornerstone of diabetes management. Utilizing blood glucose meters or continuous glucose monitoring systems allows patients to track their glucose levels in real-time. This data can guide treatment adjustments and provide valuable insights into how various factors, such as diet or exercise, influence blood sugar levels.
Moreover, the support provided by healthcare professionals cannot be overstated. Physicians, endocrinologists, diabetes educators, and mental health professionals are crucial in providing a framework for understanding and managing diabetes. Recent advancements in diabetes technology, including smart insulin pens and mobile health applications, enhance patient engagement by allowing easier tracking and management of their condition. These tools collectively enable a proactive approach to diabetes care, contributing to improved quality of life and better health outcomes.
Living with Diabetes: Real Stories and Experiences
Diabetes is not just a medical condition; it is a journey that shapes the lives of millions around the globe. Within this community, individuals are navigating the intricacies of daily life while managing their health, and their stories serve as powerful reminders of resilience and hope. One particular individual, Sarah, diagnosed at age 30, speaks candidly about the emotional rollercoaster that accompanies her routine. Initially overwhelmed by the diagnosis, she found solace in online forums where she connected with others facing similar challenges. These interactions helped her shift her perspective from feeling isolated to nurturing a sense of belonging.
Another poignant story comes from James, who has lived with type 1 diabetes since childhood. He recalls experiences of managing blood sugar levels during school events, sports, and social gatherings. Despite the hurdles, James emphasizes the importance of educating friends and family about his condition. His proactive approach not only fosters understanding but also creates a supportive environment that encourages open dialogue. Through his narrative, James highlights that embracing diabetes as a part of life rather than viewing it as a limitation can lead to personal empowerment.
Moreover, for Emma, a mother of two living with type 2 diabetes, the challenge lies in balancing her health with family responsibilities. She shares her journey of trial and error, navigating meal planning and exercise while managing busy schedules. Emma’s story showcases the importance of community support, emphasizing how local diabetes support groups provide not only resources but also emotional encouragement. These networks help individuals like Emma feel less alone and more understood in their daily battles.
Ultimately, these stories illuminate the contrasting experiences of those living with diabetes, revealing the emotional highs and lows intertwined in their lives. By sharing these personal narratives, we bridge the gap between statistics and real human experiences, fostering sympathy and understanding among readers who may be indirectly affected by diabetes.